Home care is breaking. Medicaid waitlists stretch longer every month.
Schedulers burn out faster than 911 dispatchers. Clients lose coverage because one form got filed a day late. And somewhere in the chaos, a caregiver is driving across town to a shift that got canceled two hours ago.
AI can change all of this. The question isn't whether you'll adopt it—everyone will. The question is whether you'll use it to patch the old way of doing things, or to build something fundamentally new.
This is the choice every home care provider now faces. And like a famous scene from a my favorite film, it comes down to two pills.
🔵 Take the blue pill, and AI becomes a better toolbelt for your admin team. Your schedulers still log into the EMR every morning. They still wake up on Saturdays to a flood of texts from caregivers calling out. The work gets a little faster, a little easier—but it's still the same work, done by the same people, hitting the same ceiling.
🟠 Take the orange pill, and AI stops assisting your operations. It starts running them. Calls get answered on the first ring, every time. Compliance doesn't slip through cracks because there are no cracks. Your people stop firefighting and start building—growing census, deepening referral relationships, actually talking to patients.
The blue pill measures quality the old way: a human voice on every call, even if half go to voicemail. Manual processes, because that's how it's always been done. A patchwork of vendors held together with duct tape and good intentions.
The orange pill measures quality differently: total capacity to deliver care. Zero dropped calls. Zero missed authorizations. Zero hours lost to screens when they could be spent with patients.
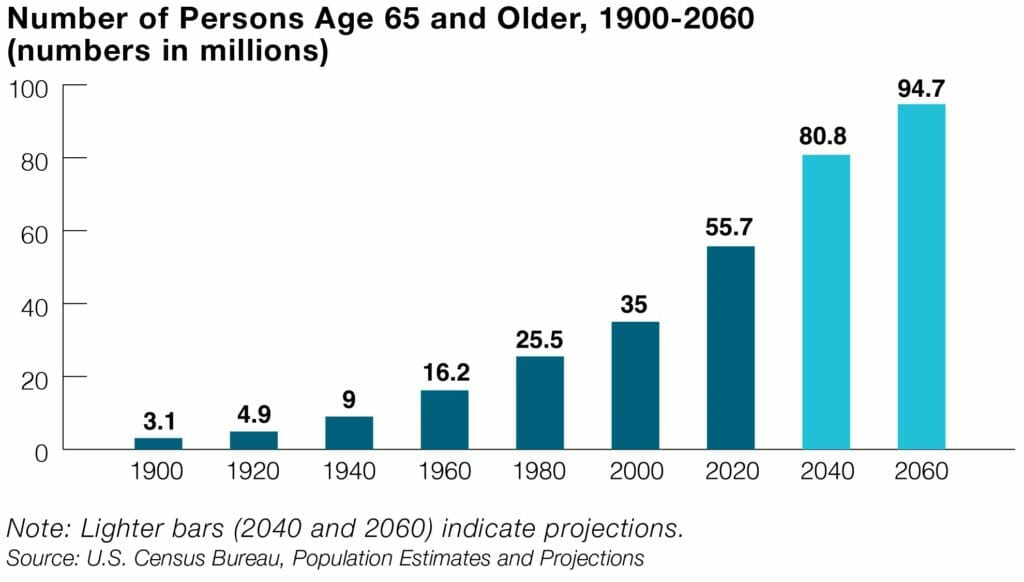
We're entering an era of accelerated pressure. By 2030, one in five Americans will be 65 or older—and the population of potential caregivers will have grown by just 1%. Meanwhile, Medicaid Fraud Control Units recovered $1.4 billion in 2024 alone, with personal care attendants accounting for 36% of fraud convictions. EVV mandates, billing audits, eligibility reviews—the compliance burden isn't shrinking. It's compounding.
The agencies that survive will be the ones whose operations can scale without adding headcount for every new patient.
The choice is yours. But we know which pill we'd take.

